
By Sarah Marquart
Medical crash carts — stocked with medications, syringes, gauze, and IV fluids — are essential tools in emergency rooms, where seconds matter, space is tight, and confusion can cost lives. However, despite their importance, crash carts vary widely in layout between hospitals and departments. In high-stress situations, this inconsistency can lead to delays as providers search for supplies or open the wrong drawers.
That’s why a team of Cornell researchers set out to reimagine the traditional crash cart, transforming it into a robot designed to support, not disrupt, emergency care teams during critical, time-sensitive procedures.
Their work, led by Angelique Taylor, assistant professor of information science at Cornell Tech, was presented in February 2025 at the ACM/IEEE International Conference on Human-Robot Interaction (HRI). The team’s paper, “Rapidly Built Medical Crash Cart! Lessons Learned and Impacts on High-Stakes Team Collaboration in the Emergency Room,” shares insights from a multi-year effort to design, prototype, and evaluate a robotic, remotely-operated version of the traditional crash cart.
As Taylor explains, the goal wasn’t to introduce entirely new equipment, but to rethink how existing tools could better support teamwork in high-pressure care settings.
“The medical crash cart robot is a cart-based platform designed to support team collaboration during medical procedures, specifically resuscitation code procedures in Emergency Departments,” explained Taylor, who is also affiliated with the Cornell Ann S. Bowers College of Computing and Information Sciences (Bowers CIS). “We wanted to explore how existing equipment in the room can be used to support team collaboration.”
To understand how this robot could function in real-life scenarios, the team designed and tested three versions of the cart-based platform. Each prototype was designed to address a core question: How can a robot effectively communicate, help reduce stress and workload, and support teams during critical care?
One significant insight came from the team’s first field deployment at Base Camp, a large-scale pediatric simulation event hosted by Weill Cornell Medicine that draws over 130 healthcare professionals across the U.S. and Canada.
“We found that the robot was very helpful in reducing mental, temporal, and physical demands,” Taylor said. “But then in terms of frustration, we did not see a reduction.”
That disconnect led the team to dig deeper into how healthcare workers understood the robot’s behavior, particularly when it opened drawers to suggest supplies. Even though participants had been briefed ahead of time, the stress of the scenario left many unsure of the reasons behind the robot’s decisions.
“The robot needed a very clear and direct way of communicating its intentions to the team,” said Taylor.
In response, the team added new ways for the robot to communicate. In subsequent prototypes, they added LED light strips as a visual cue of which drawer the robot was recommending for supply retrieval, and experimented with speech-based guidance to offer task reminders and supply locations. They also conducted lab-based studies with 84 participants to evaluate object search guidance and verbal task reminders.
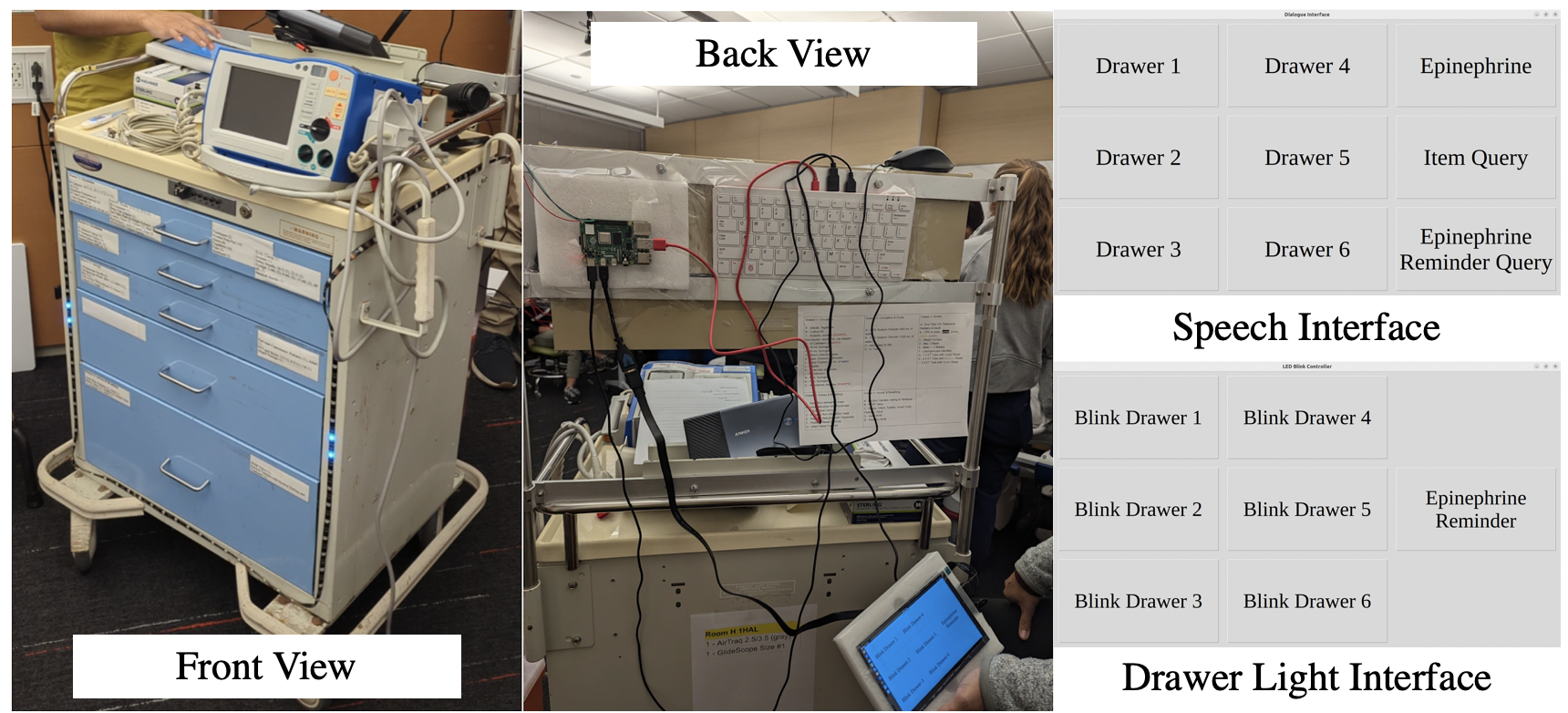
One discovery: positioning matters. Visual cues were only effective for people directly in front of the cart. Meanwhile, speech could reach more team members, but not always clearly.
“The environments are often very loud,” Taylor said. “So many times, the participants couldn’t even hear what the robot was saying.”
Long or vague spoken messages added to the challenge. Taylor noted that participants often became frustrated when the robot’s speech cues weren’t direct enough. In response, the team refined the robot’s spoken instructions to make them as concise and straightforward as possible.
Building on what they learned from these early deployments, the team is now exploring how robotic crash carts could support medical training and hospital-wide coordination. A multi-site study is currently underway to inform future iterations of the robot.
This project brought together a cross-institutional team of designers, engineers, and healthcare experts. Taylor’s team — including assistant professor Thijs Roumen of Cornell Tech and Cornell Bowers CIS; Ph.D. students Tauhid Tanjim and Michael Joseph Sack; research assistant Kexin Cheng; and Cornell Bowers CIS Associate Professor Malte F. Jung — collaborated closely with Dr. Kevin Ching and Dr. Jonathan St. George of Weill Cornell Medicine. The project also benefited from the contributions of Maia Hirsch, of the Mechanical Engineering Department at the Israel Institute of Technology, and Hee Rin Lee, of Michigan State University.
As healthcare systems face rising burnout and complexity, the team’s research offers a broader takeaway: thoughtful design can do more than assist in a crisis — it can reshape how teams communicate, coordinate, and care.
Sarah Marquart is a freelance writer for Cornell Tech.
Media Highlights
Tech Policy Press
Content Moderation, Encryption, and the LawRELATED STORIES





